| |
|
|
|
|
|
 |
| |
|
디큐펜맥스정500mg(아세트아미노펜) D Q Pen Max Tab. 500mg
|
|
일반의약품 | 비급여
|
|
|
| |
 |
알림: |
드럭인포에서는 의약품 인터넷 판매를 하지 않습니다. |
|




|
|
|
|
|
|
 |
|
|
|
|
|
|
|
|
|
|
유료회원 결재시에는 보다 다양한 약물정보를
이용하실 수 있습니다.
유료정보목록은 전문회원으로
로그인 하시면 확인 가능합니다.
|
|
|
 | 허가정보 |
|
|
| 항목 |
내용 |
청구코드(KD코드)
비급여점검코드
상한금액 |
661605740
[보험코드에 따른 약품기본정보 직접조회]
[비급여]
[상병코드조회]
[질병코드조회]
|
| 빠른조회 |
|
| 제품성상 |
흰색의 장방형 필름코팅정제 [제형정보 확인] |
| 포장·유통단위 |
10 정/상자(10정/피티피),30 정/병
|
| 포장·코드단위 |
| 약품규격 |
단위 |
포장형태 |
대표코드 |
표준코드 |
비고 |
| 500밀리그램 |
30 정 |
병 |
8806616057405 |
8806616057412 |
|
|
| 주성분코드 |
101305ATB
[동일한 주성분코드를 가진 오리지날 또는 제네릭 의약품 조회]
|
| 허가사항 원문조회 |
[허가사항 원문조회]
|
| 효능효과 |
[적응증 별 검색]


1. 주효능·효과
감기로 인한 발열 및 동통(통증), 두통, 신경통, 근육통, 월경통, 염좌통(삔 통증)
2. 다음 질환에도 사용할 수 있다.
치통, 관절통, 류마티양 동통(통증)
|
| 1일 최대 투여량 |
유료정보입니다.
|
| 약물음식간 상호작용 |
[조회]
|
| 용법용량 |
* 절대 임의복용하지 마시고 반드시 의사 또는 약사와 상담하시기 바랍니다.


[처방약어]
만 12세 이상 소아 및 성인 :
1회 1~2정씩 1일 3~4회 (4~6시간 마다) 필요시 복용한다.
1일 최대 4g(8정)을 초과하여 복용하지 않는다.
이 약은 가능한 최단기간동안 최소 유효용량으로 복용한다.
|
| 금기 |
1) 이 약에 과민증 환자
2) 소화성궤양 환자
3) 심한 혈액 이상 환자
4) 심한 간장애 환자
5) 심한 신장(콩팥)장애 환자
6) 심한 심장기능저하 환자
7) 아스피린 천식(비스테로이드성 소염(항염)제에 의한 천식발작 유발) 또는 그 병력이 있는 환자
8) 다음의 약물을 복용한 환자 : 바르비탈계 약물, 삼환계 항우울제
9) 알코올을 복용한 사람
|
| 신중투여 |
1) 간장애 또는 그 병력이 있는 환자
2) 신장(콩팥)장애 또는 그 병력이 있는 환자
3) 소화성궤양의 병력이 있는 환자
4) 혈액이상 또는 그 병력이 있는 환자
5) 출혈경향이 있는 환자(혈소판기능이상이 나타날 수 있다.)
6) 심장기능이상이 있는 환자
7) 과민증의 병력이 있는 환자
8) 기관지 천식 환자
9) 고령자(노인)
10) 임부 또는 수유부
11) 와파린을 장기복용하는 환자
12) 다음의 약물을 용한 환자 : 리튬, 치아짓계이뇨제
|
| 이상반응 |
다음과 같을 경우 이 약의 복용을 즉각 중지하고 의사, 치과의사, 약사와 상의할 것. 상담시 가능한 한 이 첨부문서를 소지할 것
1) 쇽: 쇽, 아나필락시양 증상 (과민성유사증상 : 호흡곤란, 온몸이 붉어짐, 혈관부기, 두드러기 등), 천식발작
2) 혈액: 혈소판 감소, 과립구감소, 용혈성(적혈구 파괴성)빈혈, 메트헤모글로빈혈증, 혈소판기능 저하(출혈시간 연장), 청색증
3) 과민증: 과민증상(얼굴부기, 호흡곤란, 땀이 남, 저혈압, 쇽)
4) 소화기: 구역, 구토, 식욕부진, 장기복용시 위장출혈, 소화성궤양, 천공(뚫림) 등의 위장관계 이상반응
5) 피부: 발진, 알레르기 반응, 피부점막안 증후군(스티븐스-존슨 증후군), 중독성표피괴사용해(리엘 증후군)
6) 대사 및 영양장애: 고음이온차 대사성 산증(HAGMA)
7) 기타: 장기투여시 만성간괴사, 급성췌장(이자)염, 만성간염, 신장(콩팥)독성
8) 과량투여: 간장, 신장(콩팥), 심근의 괴사
9) 이 약에 대해 시판 후 조사에서 보고된 추가적 이상반응은 아래 표와 같다. 발현빈도는 매우 흔히 ≥1/10, 흔히 ≥1/100 및 <1/10, 흔하지 않게 ≥1/1,000 및 <1/100, 드물게 ≥1/10,000 및 <1/1,000, 매우 드물게 <1/10,000 이다.
| 면역계 장애 매우 드물게 : 아나필락시스 반응, 과민증 피부 및 피하(피부밑)조직 장애 매우 드물게 : 두드러기, 소양성(가려움) 발진, 발진, 고정발진 |
표. 자발적 보고율로부터 추정한 빈도에 따른 이 약의 시판후 경험에서 밝혀진 이상반응
10) 국내 부작용 보고자료의 분석·평가에 따라 다음의 이상반응을 추가한다.
● 간담도계: AST 상승, ALT 상승
● 피부: 고정발진
|
|
|
 | 정보요약 |
|
|
|
드럭인포 의약품 요약/상세정보
|
|
 | 코드 및 분류정보 |
|
|
| |
|
 | 제품정보 |
|
|
|
|
 | 복약정보 |
|
|
| 항목 |
내용 |
| LACTmed 바로가기 |
[바로가기]
|
| 약리작용 |
유료정보입니다.
|
| 축약복약지도 |
유료정보입니다.
|
| 복약지도 |
유료정보입니다.
|
| 임부에대한투여 |
| * |
전체임신 기간별로 여러등급이 존재할 수 있으며 가장 위험도가 높은 정보만 보여집니다. 단, 복합제의 경우 모든 복합제성분에 대한 임부투여등급이 표시된것은 절대 아니며 표시된것중에 가장 위험도가 높은 정보만 나타납니다.
|
|
| |

FDA : B등급
|



|
| * |
상기 임부투여에 대한 정보는 전산처리 되면서 입력 오류 가능성이 존재합니다. 오류 가능성을 최소화하기 위하여 많은 노력을 기울이고 있으나, 그 정확성에 대하여 확신을 드릴 수 없습니다. 이에 대해 회사는 책임을 지지 않습니다.
|
| * |
반드시 공신력 있는 문헌을 다시 한번 참고 하시기 바라며 의사 또는 약사의 판단에 따라 투여여부가 결정되어야 합니다.
|
|
|
신장애, 간장애시
용량조절 |
유료정보입니다.
|
| Pharmacokinetics |
유료정보입니다.
|
| 보관상 주의 |
|
| 조제시 주의 |
|
|
|
 | 심사정보 |
|
|
|
|
 | 학술정보 |
|
|
| 항목 |
내용 |
| DUR (의약품사용평가) |
병용금기 :
고시된 병용금기 내용은 없습니다.
[상호작용/병용금기검색]
연령대금기 :
고시된 연령금기 내용은 없습니다.
[연령대금기상세검색]



|
| 화학구조 및 물성 |
[Acetaminophen]
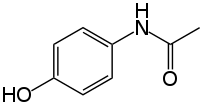
[Acetaminophen]
CAS number/103-90-2
ATC code/N02BE01
PubChem/1983
DrugBank/APRD00252
Formula/C8H9NO2
Mol. mass/151.17 g/mol
Bioavailability/almost 100%
Metabolism/90 to 95% Hepatic
Excretion/Renal
Pregnancy cat./
A(AU) B(US) safe
Legal status/
Unscheduled(AU) GSL(UK) OTC(US)
Routes/Oral, rectal, intravenous
Solubility/1.4쟥/100쟭l or 14쟭g/mL (20젾C)
|
| 독성정보 |
Acetaminophen에 대한 독성정보 : 정보보기
출처: 국립독성과학원 독성물질정보DB : http://www.nitr.go.kr/nitr/contents/m134200/view.do |
| Mechanism of Action |
Acetaminophen에 대한 Mechanism_Of_Action 정보
Acetaminophen is thought to act primarily in the CNS, increasing the pain threshold by inhibiting both isoforms of cyclooxygenase, COX-1 and COX-2, enzymes involved in prostaglandin (PG) synthesis. Unlike NSAIDs, acetaminophen does not inhibit cyclooxygenase in peripheral tissues and, thus, has no peripheral anti-inflammatory affects. While aspirin acts as an irreversible inhibitor of COX and directly blocks the enzyme's active site, studies have found that acetaminophen indirectly blocks COX, and that this blockade is ineffective in the presence of peroxides. This might explain why acetaminophen is effective in the central nervous system and in endothelial cells but not in platelets and immune cells which have high levels of peroxides. Studies also report data suggesting that acetaminophen selectively blocks a variant of the COX enzyme that is different from the known variants COX-1 and COX-2. This enzyme is now referred to as COX-3. Its exact mechanism of action is still poorly understood, but future research may provide further insight into how it works.
|
| Pharmacology |
Acetaminophen에 대한 Pharmacology 정보
Acetaminophen (USAN) or Paracetamol (INN) is a popular analgesic and antipyretic drug that is used for the relief of fever, headaches, and other minor aches and pains. It is a major ingredient in numerous cold and flu medications and many prescription analgesics. It is extremely safe in standard doses, but because of its wide availability, deliberate or accidental overdoses are not uncommon. Acetaminophen, unlike other common analgesics such as aspirin and ibuprofen, has no anti-inflammatory properties or effects on platelet function, and so it is not a member of the class of drugs known as non-steroidal anti-inflammatory drugs or NSAIDs. In normal doses acetaminophen does not irritate the lining of the stomach nor affect blood coagulation, the kidneys, or the fetal ductus arteriosus (as NSAIDs can). Like NSAIDs and unlike opioid analgesics, acetaminophen does not cause euphoria or alter mood in any way. Acetaminophen and NSAIDs have the benefit of being completely free of problems with addiction, dependence, tolerance and withdrawal. Acetaminophen is used on its own or in combination with pseudoephedrine, dextromethorphan, chlorpheniramine, diphenhydramine, doxylamine, codeine, hydrocodone, or oxycodone.
|
| Metabolism |
Acetaminophen에 대한 Metabolism 정보
# Phase_1_Metabolizing_Enzyme:Cytochrome P450 1A2 (CYP1A2)Cytochrome P450 2E1 (CYP2E1)
|
| Half-life |
Acetaminophen에 대한 반감기 정보
1 to 4 hours
|
| Absorption |
Acetaminophen에 대한 Absorption 정보
Rapid and almost complete
|
| Pharmacokinetics |
Acetaminophen의 약물동력학자료
- 단백결합 : 20-50%
- 대사 :
- 상용량에서 : 간에서 sulfate와 glucuronide 포합체로 대사되며, 소량은 microsomal mixed function oxidases에 의해 반응성이 매우 높은 중간대사체(acetylimidoquinone)로 대사된 후 glutathione 포합으로 비활성화된다.
- 중독량에서 (4g을 단 하루 복용한 정도까지도 포함된다) : glutathione 포합이 점점 불충분하게 되어 acetylimidoquinone 농도가 증가하게 되며 이것이 간세포 괴사를 유발하는 것으로 여겨지고 있다.
- 반감기
- 신생아 : 2-5 시간
- 성인
- 정상 신기능 : 1-3 시간
- 말기 신질환 : 1-3 시간
- 최대혈중농도 도달시간
- 경구 : 상용량 복용시 10-60분, 급성 중독량 복용시 지연될 수 있다.
|
| Biotransformation |
Acetaminophen에 대한 Biotransformation 정보
Approximately 90 to 95% of a dose is metabolized in the liver via the cytochrome P450 enzyme pathways (primarily by conjugation with glucuronic acid, sulfuric acid, and cysteine). An intermediate metabolite is hepatotoxic and most likely nephrotoxic and can accumulate after the primary metabolic pathways have been saturated.
|
| Toxicity |
Acetaminophen에 대한 Toxicity 정보
Oral, mouse: LD50 = 338 mg/kg; Oral, rat: LD50 = 1944 mg/kg. Acetaminophen is metabolized primarily in the liver, where most of it is converted to inactive compounds by conjugation with sulfate and glucuronide, and then excreted by the kidneys. Only a small portion is metabolized via the hepatic cytochrome P450 enzyme system. The toxic effects of acetaminophen are due to a minor alkylating metabolite (N-acetyl-p-benzo-quinone imine), not acetaminophen itself nor any of the major metabolites. This toxic metabolite reacts with sulfhydryl groups. At usual doses, it is quickly detoxified by combining irreversibly with the sulfhydryl group of glutathione to produce a non-toxic conjugate that is eventually excreted by the kidneys. The toxic dose of paracetamol is highly variable. In adults, single doses above 10 grams or 140 mg/kg have a reasonable likelihood of causing toxicity. In adults, single doses of more than 25 grams have a high risk of lethality.
|
| Drug Interactions |
Acetaminophen에 대한 Drug_Interactions 정보
Anisindione Acetaminophen increases the anticoagulant effectWarfarin Acetaminophen increases the anticoagulant effectImatinib Increased hepatic toxicity of both agentsIsoniazid Risk of hepatotoxicityDicumarol Acetaminophen increases the anticoagulant effectDicumarol Increases the anticoagulant effectAcenocoumarol Increases the anticoagulant effect
|
CYP450
Drug Interaction |
[CYP450 Table직접조회]
Acetaminophen에 대한 P450 table
SUBSTRATES
CYP 2E1
**acetaminophen**
chlorzoxazone
ethanol
INHIBITORS
CYP 2E1
disulfiram
INDUCERS
CYP 2E1
ethanol
isoniazid
|
| Food Interaction |
Acetaminophen에 대한 Food Interaction 정보
Take without regard to meals.Avoid alcohol (may increase risk of hepatotoxicity).
|
| Drug Target |
[Drug Target]
|
| Description |
Acetaminophen에 대한 Description 정보
Analgesic antipyretic derivative of acetanilide. It has weak anti-inflammatory properties and is used as a common analgesic, but may cause liver, blood cell, and kidney damage. [PubChem]
|
| Drug Category |
Acetaminophen에 대한 Drug_Category 정보
Analgesics, Non-NarcoticAntipyretics
|
| Smiles String Canonical |
Acetaminophen에 대한 Smiles_String_canonical 정보
CC(=O)NC1=CC=C(O)C=C1
|
| Smiles String Isomeric |
Acetaminophen에 대한 Smiles_String_isomeric 정보
CC(=O)NC1=CC=C(O)C=C1
|
| InChI Identifier |
Acetaminophen에 대한 InChI_Identifier 정보
InChI=1/C8H9NO2/c1-6(10)9-7-2-4-8(11)5-3-7/h2-5,11H,1H3,(H,9,10)/f/h9H
|
| Chemical IUPAC Name |
Acetaminophen에 대한 Chemical_IUPAC_Name 정보
N-(4-hydroxyphenyl)acetamide
|
| Drug-Induced Toxicity Related Proteins |
ACETAMINOPHEN 의 Drug-Induced Toxicity Related Protein정보
Replated Protein:Alpha-2A adrenergic receptor
Drug:acetaminophen
Toxicity:hepatic injury .
[바로가기]
Replated Protein:Myeloperoxidase
Drug:acetaminophen
Toxicity:respiratory burst.
[바로가기]
Replated Protein:Glucose-6-phosphate 1-dehydrogenase
Drug:acetaminophen
Toxicity:drug-induced hemolysis.
[바로가기]
Replated Protein:Ornithine decarboxylase
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Lactate dehydrogenase
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Transcription factor AP-1(JUN)
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Haptoglobin
Drug:acetaminophen
Toxicity:drug-induced hemolysis.
[바로가기]
Replated Protein:Alanine aminotransferase
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Beta-glucuronidase
Drug:acetaminophen
Toxicity:hepatotoxin-induced effects.
[바로가기]
Replated Protein:CYP2E1
Drug:Acetaminophen
Toxicity:idiosyncratic hepatotoxicity.
[바로가기]
Replated Protein:Cytochrome P450 2E1
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Sulfotransferase family cytosolic
Drug:acetaminophen
Toxicity:chronic hypoxia.
[바로가기]
Replated Protein:Cytochrome P450 3A4
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Caspase recruitment domain-containing protein
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
Replated Protein:Cytochrome P450 1A2
Drug:acetaminophen
Toxicity:hepatotoxicity.
[바로가기]
ACETAMINOPHEN (APAP) 의 Drug-Induced Toxicity Related Protein정보
Replated Protein:Cytochrome P450
Drug:acetaminophen (APAP)
Toxicity:renal functional changes, strain-dependent histopathological changes.
[바로가기]
|
|
|
 | 사용자컨텐츠 |
|
|
|
|
|
-
최근정보수정일 2025-11-12
-
본 수정일 정보는 허가정보 이외의 기타정보 수정일을 의미하므로, 허가정보수정일은 본문에 표기된 날짜를 참조하시기 바랍니다.
|
|
 알림 알림 |
상세정보는 식품의약품안전처의 제품허가사항을 토대로 작성되었으며 요약정보는 상세정보 및 기타문헌을 기반으로 드럭인포에서 편집한 내용입니다. 제품허가사항의 목차와 다소 상이할 수 있습니다. |
|
 경고 경고 |
드럭인포 의약학술정보는 식품의약품안전처의 제품허가사항, 학술문헌, 제약회사 제공정보 등을 근거로 작성된 참고 정보입니다.
정보의 정확성을 위해 노력하고 있으나 편집상의 오류, 허가사항 변경, 추가적인 학술연구 또는 임상연구 발표 등으로 인해 발생하는 문제에 대해 드럭인포는
책임을 지지 않습니다. 자세한 내용은 “책임의 한계 및 법적고지”를 참조해 주십시오.
반드시 제조·수입사, 판매사, 의사, 약사에게 최종적으로 확인하시기 바랍니다.
전화: 02-3486-1061 ㅣ 이메일: webmaster@druginfo.co.kr
|
|
아래의 내용을 포함한 전체 데이터를 보시려면
여기로 이동하시기 바랍니다.
The database contains the following fields: The generic name of each chemical For module A10 (liver enzyme composite module): Overall activity category for each compound (A for active, M for marginally active, or I for inactive) based on the number of active and marginally active scores for each compound at the five individual endpoints (see research article for full description of method) Number of endpoints at which each compound is marginally active (M) Number of endpoints at which each compound is active (A) For modules A11 to A15 (alkaline phosphatase increased, SGOT increased, SGPT increased, LDH increased, and GGT increased, respectively): Overall activity category for each compound (A for active, M for marginally active, or I for inactive) based on the RI and ADR values (see the research article for full description of method) Number of ADR reports for each compound, given as <4 or ≥4 Reporting Index value for each compound, except where no shipping units were available (NSU) Group 1 comprises of compounds for which ADR data were available for the first five years of marketing, so when no ADR reports were listed during this period the compounds were evaluated as inactive. Group 2 comprises of compounds for which a 'steady state' period of ADR data were available (1992-1996). In cases where no ADR reports were filed during this period, the compounds were scored as 'NA' (data not available) since they may have had one or more ADR reports during their first five years of marketing which should not be negated by a lack of ADR reports during the steady-state period. ACETAMINOPHEN[Composite Activity](Score) A(Marginal) 3(Active) 2[Alkaline Phosphatase Increase](Activity Score) M(Number of Rpts) ≥4(Index value) NSU[SGOT Increase](Activity Score) A(Number of Rpts) ≥4(Index value) NSU[SGPT Increase](Activity Score) A(Number of Rpts) ≥4(Index value) NSU[LDH Increase](Activity Score) M(Number of Rpts) ≥4(Index value) NSU[GGT Increase](Activity Score) M(Number of Rpts) ≥4(Index value) NSU
병용금기 및 특정연령대 금기 성분
|
|
|
|